What is Prediabetes?
To mark the Diabetes (Type-2) Prevention Week, we shall provide you with a brief overview of what prediabetes is, why it is significant, who is most at risk and what can be done to tackle it.
What is prediabetes?
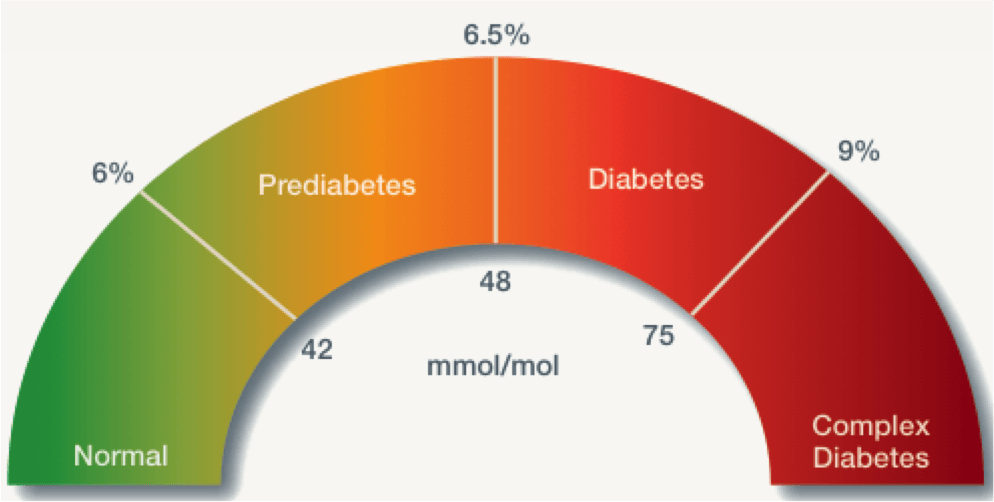
Prediabetes, also known as non-diabetic hyperglycaemia, is a serious health condition that sees a person’s blood glucose level reside above the healthy range, but reside just below the range required for the person to be diagnosed with Type-2 Diabetes (T2D).
An individual is deemed prediabetic if they have an HbA1c reading of between 42mmol/mol (6%) to 47.9mmol/mol (6.4%) or a fasting plasma glucose (FPG) of 5.5mmol/l to 6.9 mmol/l.
In the UK, statistics suggest that there are 13.6 million people at risk of developing Type-2 diabetes.
Why is prediabetes important?
Yes, prediabetes is indeed incredibly important with a multitude of reasons as to why it is significant. We shall present you with the leading two. Firstly, prediabetes is effectively silent. Prediabetes generally does not present with any symptoms, meaning that the person is unaware they have a clinically high chance of progressing onto developing T2D. An individual deemed prediabetic may also be at risk of developing metabolic syndrome. Metabolic syndrome is defined as a syndrome that includes a cluster of common pathologies: obesity, insulin resistance dyslipidemia and hypertension.1 Sadly, by the time an individual is made aware they are diabetic, specifically T2D, they would have most likely succumb to a cardiovascular event such as a stroke or a myocardial infraction. At this point they may, depending on the severity, experience a marked reduction in their quality of life. The patient’s diminished quality of life also impacts the NHS financially.

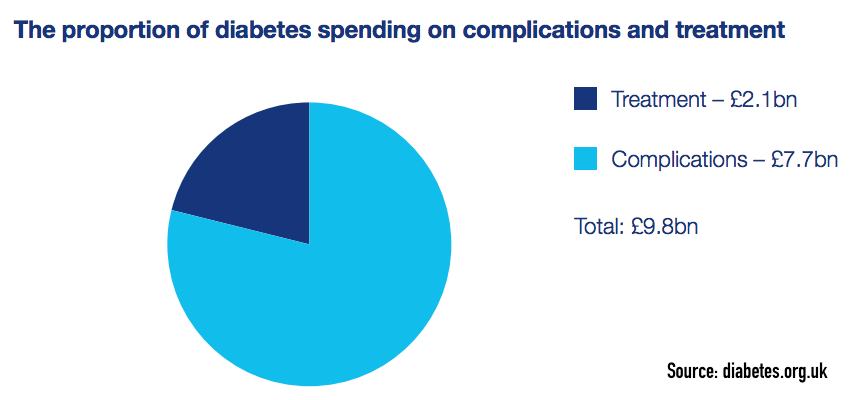
The second significant reason is the cost on the NHS to treat a patient now diabetic as a result of no clinical intervention taking place earlier on in the patient’s therapeutic journey. The annual cost of diabetes to the NHS stands at approximately £14bn a year.2 NHS spending on diabetic complications and treatment equates to £2.1bn and £7.7bn respectively.
As of 2019, there were 3.9 million people living with a diagnosis of diabetes in of which, 90% of those are type 2. This is to say nothing of the undiagnosed 1 million people living with Type-2 diabetes or those who are prediabetes. In the UK, it is projected that incidences of diabetes will rise with 5.5 million living with some form of the condition by 2030.
From the current data and the projected forecasts it is vital that we do everything we can both be it individually or as a company to support the reduction of clinical and financial pressure on the NHS as a result of the rising incidences of Type-2 diabetes diagnosis. To protect both patients and the NHS, in particularly primary care, the application of the old adage “prevention is better than cure” is most applicable and welcomed.
Who is most at risk of prediabetes?
You are most at risk of prediabetes and the subsequent risk of developing T2D if:
- You’re white and over 40 or over 25 if you’re African-Caribbean, Black African, or South Asian.
- You are of South Asian descent and African-Caribbean or Black African descent, as T2D is two to four times more likely in people of these ethnicities.
- You have a family history of T2D. You are two to six times more likely to develop type 2 diabetes if you have a parent, brother, sister or child with diabetes.
- You’ve ever had high blood pressure.
- You are carrying extra weight, especially if this weight is around your midriff & lower belly.
It is estimated that 5%-10% of pre-diabetic patients will become diabetic each year with a similar percent reverting back to normoglycaemia.5
This offers a glimmer of hope and an opportunity to prevent developing metabolic syndrome or T2D by taking the initiative to make the necessary inteventions early on.
To start you journey of prevention today. Consider using the Know your risk Type-2 Diabetes by clicking this link:
https://preventing-diabetes.co.uk/Know-your-risk-dtc/

How do you treat Prediabetes, what can be done?
As mentioned above, prediabetes is preventable and reversible if identified early. The first thing you can do if you identify as a high risk patient for prediabetes or T2D is to speak with your GP surgery to arrange for a blood test. This blood test will measure you HbA1c levels for the last two to three months.
Another step you can take to reverse your prediabtes and reduce your chances of developing type to diabetes is to focus on improving your nutrition and increasing your physical activity. With nutrition the aim here is not to strave yourself but to make better choice that are low in sugar (simple carbohydrates) and reasonable portions of complex carbohydrates. This links well into increasing levels of exercise and physical activity. The link and the objective with exercise, is to ensure your level of energy expenditure is greater than your calorific intake.
You can begin to implement these changes yourself, or better yet, for more effective guidance and results ask your GP surgery about the NHS Diabetes Prevention Programme (NDPP). Please see links below for further information.

© All rights reserved, Nnadi’s Healthcare & Pharmaceuticals Limited, 2022.
Signposting:
NHS Diabetes Prevention Programme (NDPP): https://www.england.nhs.uk/diabetes/diabetes-prevention/
Know Your Risk Tool: https://preventing-diabetes.co.uk/Know-your-risk-dtc/ .
Xyla Health & Wellbeing: https://xylahealthandwellbeing.com/contact-us/
Reference:
1.Basciano H, Federico L and Adeli K. Fructose, insulin resistance, and metabolic dyslipidemia. Nutr & Metab. 2005. 2:5, 1-14.
NHS Diabetes Prevention Programme (NDPP): https://www.england.nhs.uk/diabetes/diabetes-prevention/
2. Kanavos, Van den Aardweg and Schurer: Diabetes expenditure, burden of disease and management in 5 EU countries. 2012. LSE.
3. Diabetes UK. Diabetes Statistics. < https://www.diabetes.org.uk/professionals/position-statements-reports/statistics > accessed 08th May 2022.
4. Diabetes UK. Prediabetes. < https://www.diabetes.org.uk/preventing-type-2-diabetes/prediabetes >
5. Twohig H. Hodges V. Mitchell C. Editorial Prediabetes: Opportunity or Overdiagnosis. Brit. J. Gen Pract. 172-173.