COVID-19 Series PART II
14 September 2020
COVID-19 Series, PART II: Holistic approaches against COVID-19. What you can do.
As explained in Part I of our series, it is apparent that the main objective for clinical staff in the fight against COVID-19 is avoid the patient’s condition progressing from the viral phase to the pulmonary phase and then to the dreaded severe phase. It is this final stage that unleashes a devastating autoimmune reaction that exponentially raises the chances of the patient fatally succumbing to COVID-19. Amongst the clinical healthcare professionals (HCP) there resides a very much founded fear and sense of urgency to protect patients with pre-existing endothelial dysfunction and other physiological risk factors (being a male, diabetics and obese etc.) from the inflammatory response due to endotheliitis (inflammation of the endothelial lining). The key take home messages from Part I, based on the accounts of front line doctors, is that COVID-19 “is not just a little flu” and that preventative measures are still the most effective approaches in dealing with this pandemic. This part of the series look at the holistic approaches you can adopt and hopefully answers the question of what you can do to protect yourself and others.
The Basics: Hygienic & Social Practices.
Hand-washing, as simple as the activity is, proved to be revolutionary in the fight against microorganisms and viral pathogens. Just as this practice was much welcomed in the 1800’s, it is even more so and highly effective in 2020. Hand-washing with soap is more efficacious than the use of alcohol or disrespectful. Scientifically, soap is effective because the COVID-19 virus is self-assembled nanoparticle in which the weakest link is the lipid (fatty) bilayer. In simple terms the soap outcompetes on two fronts. Firstly, the soap, due to its fat-like substances known as amphiphiles (possessing both water loving and water hating properties), of which some are structurally similar to the lipids in the virus membrane, is able to compete with the said lipids in the viral membrane. Soap competes with non-covalent bonds that help bind the protein, viral RNA and lipids together. Thus, soap effectively “dissolves” the “glue” holding the virus together. All that is required after this point is water completely destroy the virus. Secondly, soap molecules are able to compete with the interactions between the virus and the skin surface. Soon the virus becomes detached and falls apart due to the combined action of the soap and water 1
. Numerous studies present irrefutable evidence from their findings on the efficaciousness of hand-washing. The most poignant and relevant to our argument are these two points. Firstly, a million deaths a year could be prevented if everyone routinely washed their hands 2
. Secondly, that hand-washing reduces the risk of respiratory infections by 16% 3
.

In addition to basic hygienic practices the wearing of a mask and facial covering help enormously in reducing the transmission of COVID-19 to other individuals. According to the scientific briefing from the World Health Organization (WHO), COVID-19 is primarily transmitted between people through respiratory droplets. Hence, COVID-19 spreads by direct contact with an infected person or people and via indirect contact with surfaces in the immediate environment or with objects used on the infected person 4
.
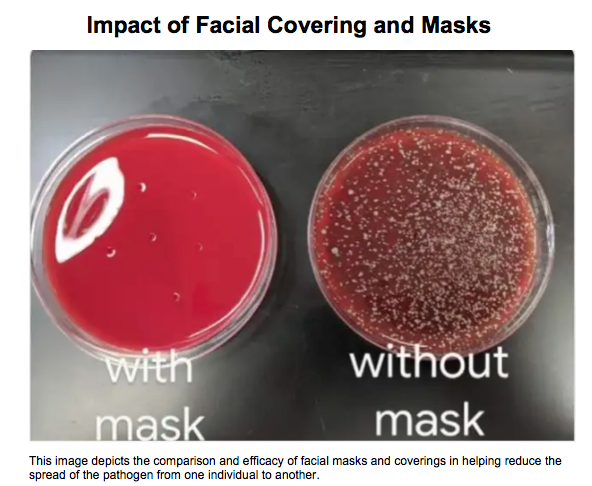
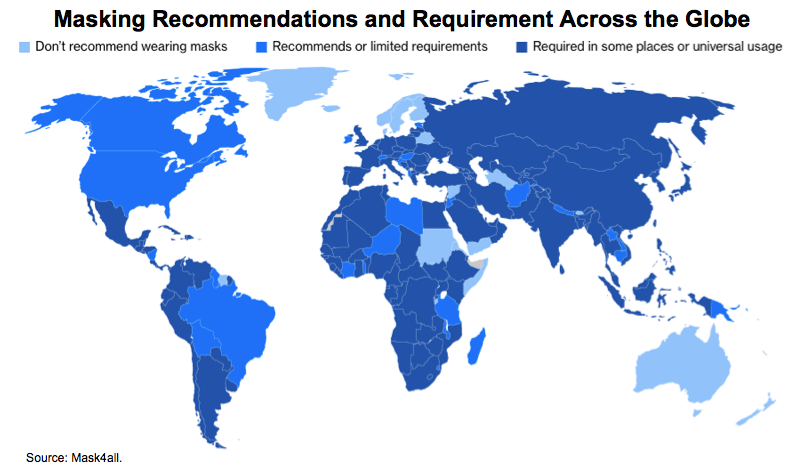
The picture above speaks for itself regarding the effects of a mask. To reiterate, the primary rationale is to minimise the spread of pathogens to others. The use of a mask and face covering is an effective tool in reducing the ‘R” rate (the viral reproduction number) from exceeding 1.0. As a result of face masks being effective and very much alignment with government’s initiative to reduce the R rate triggering a second wave, the government have now made face masks mandatory for any individual on public transport and in certain indoor settings across England and Scotland 5
. Face covering and wearing a mask is mandatory in the EU and across the globe with a total of 120 countries following suit in making masks and face covering mandatory 6
.
Another approach to minimising the spread of the pathogen is for the population to adopt and adhere to social distancing guidelines. As mentioned earlier, transmission occurs when a person is in close contact with someone who has respiratory symptoms and is therefore at risk of having his/her mucosae (mouth and nose) or conjunctiva (eyes) exposed to potentially infective respiratory droplets 7
. The argument for social distancing is validated by mathematical modelling devised by Dr. Robin Thompson, a junior research fellow mathematical epidemiologist, that demonstrated that without social distancing being observed one sufferer could in six weeks have started chains of transmission with 1093 cases. In comparison, a model with social distancing observed would see the same sufferer, in six weeks start chains of transmissions with 127 cases 8
. Therefore, a reduction in person-to-person contact reveals a scenario in which case numbers could be reduced by almost 90% through social distancing. Given that 80% of individuals who contract COVID-19 present as asymptomatic (showing no signs or symptoms associated with the disease), it exacerbates the concerns and compounds the complacency around the rate and transmission of infection. Despite scientific advances proposing hotly anticipated therapeutics, observing social distancing, facial covering and regular hand-washing with soap (preferably, but hand-gel/sanitisers can be used if soap is unavailable) are the main barriers to the virus so far. These measures are not taxing physically, they are cheap and they prove to be highly effective.
If we could conclude on a bold note, knowing what we know now about this virus so far, and the immunological devastation it can cause, a lack of consideration for each other is equally as dangerous as the COVID-19 virus itself.
Exercise & Physical Activities.
Reviewing holistic approaches that can be adopted and assessing them against the disease state of the offending pathogen, exercise and physical activity are certainty stellar and proactive holistic practices with benefits that meet and exceed immunological protection from COVID-19.
Despite exercise-immunology being considered a relatively papers on this field show that the immune system is very responsive to exercise in accordance to the extent and duration that reflects the degree of physiological stress imposed by the workload. Acute exercise, defined a moderate and vigorous intensity aerobic exercise of bouts less than 60 minutes durations enhance anti-pathogen activity of tissue macrophages (helpful large scavenger cells) as well as simultaneously increasing the recirculation of immunoglobulins, anti-inflammatory cytokines, neutrophils, NK (natural killer) cells, cytotoxic T cells and immature B cells of which play critical roles in immune defence activity and metabolic health. Simply put, acute exercise stimulates the interchange of innate immune system cells (fast effective responders and the first line of defence against germs) between lymphoid tissues and the blood compartment, with an aggregating effect over time of improved immunosurveillance against pathogens and cancer cells and decreased systemic inflammation. In general acute exercise is now viewed as an important immune system adjuvant (booster) to stimulate the ongoing exchange of leukocytes between the circulation and tissues 9
.
The real take home point with regards to encouraging the incorporation of exercise, is that sessions under 60 minutes will suffice to confer the desired and protective benefits above. Equally research has shown that overtraining and adopting intense physical exercise above 60 minutes can have deleterious effects on the individual’s immune system as a result of the physiological stress experienced by the exerciser.
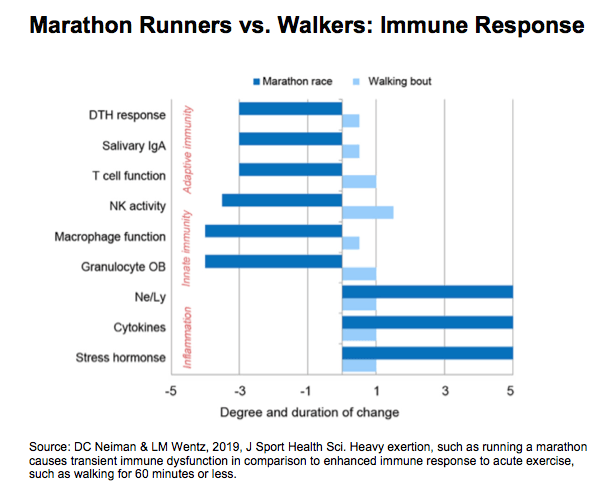
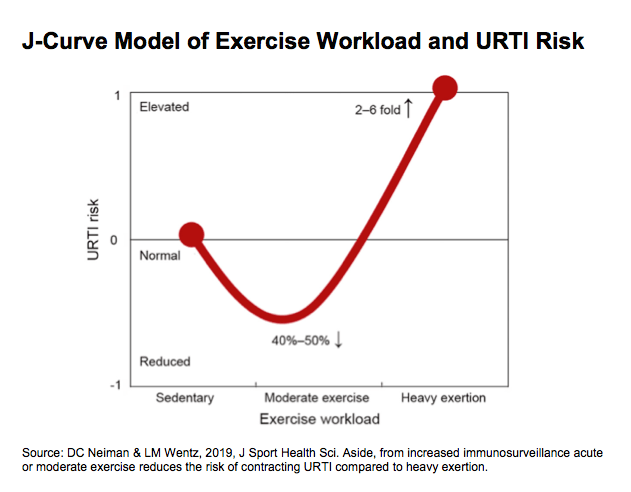
More pertinently to COVID-19, numerous randomized controlled trials (RCT) conducted to establish the relationship between exercise and upper respiratory infections (URTI), showed a reduction of URTI symptoms in those individuals who undertook moderate exercise and physical activity that ranged between average 40-50% in comparison to those who were largely sedentary. Noticeably, those who engaged in strenuous excessive and prolonged exercise experienced a 2-6 fold increase in presenting with URTI symptoms. Furthermore, epidemiological studies suggest that regular physical activity is associated with decreased mortality and incidence rates for influenza and pneumonia. Given the collective findings from the RCTs, it serves to substantiate and hopefully bolster public health guidelines urging individuals to be physically active on a regular basis.
Another risk factor aside from URTI symptoms is clinical obesity, defined as a body mass index (BMI) of above 30. Obesity is linked with persistent increases inflammation biomarkers defined as chronic or systemic inflammation. Obesity induces a constant state of low grade inflammation characterized by activation and infiltration of proinflammatory immune cells such as macrophages and granulocytes and a dysregulation of acute phase proteins reactive oxygen species (ROS) metalloproteinases, and other cell signaling molecules 10
. Regular exercise training has an overall anti-inflammatory influence mediated through multiple pathways. Numerous epidemiologic studies have shown decreased levels of inflammatory biomarkers in adults with higher levels of physical activity and fitness of which the effects are still favourable and noticeable when BMI is adjusted. Exercise/physical activity is essential along with dietary adjustments, in better managing and reducing an individual’s weight. As the most reason recent comprehensive study found that obesity increases risk of COVID-19 death by 48% and what’s more the study goes on to suggest that the vaccine may not as work as well for overweight people 11
.
The final risk factor and point regarding the benefit of exercise and physical activity is its effect on age, otherwise termed as immunosenescence. Immunosenescence defined as the gradual deterioration of the immune system brought about by the natural advancement of age. This increases the susceptibility to infections, autoimmune diseases, neoplasia’s, metabolic diseases, osteoporosis and neurologic disorders. However, this natural phenomenon can be remodelled and delayed by undertaking habitual exercise. In cross-sectional studies comparing immune function in highly conditioned and sedentary women found that the highly conditioned elderly women had significantly higher levels of NK cells and T-lymphocytes function and reduced illness rates compared with the 30 sedentary elderly women. The delaying of the onset of immunosenescence via physical exercise confer conducive physiological attributes to stave off and improve the prognosis of a COVID-19 infection by enhancing the individuals vaccination response, lowering inflammatory response to bacterial challenge and improve the NK cell activity.
Supplements, Dietary & Lifestyle Habits.
Along with basic hygienic practices social distancing and exercise, supplements, dietary and lifestyle changes have a role aiding boost or preserve an effective and responsive immune system.
Beginning with Vitamin D, fat-soluble vitamin capable of enhancing absorption of calcium in the small intestine and in doing so promotes calcium homeostasis (normal functioning) to promote bone health, a deficiency in this vitamin has been associated with an increased autoimmunity as well as an increased susceptibility to infection 12
. According to multiple cross-sectional studies carried out between 1988 to 1994 involving 19,000 subjects, which investigated the association of lower levels of vitamin D with increased infection, individuals with a lower vitamin D (<30ng/ml) were more likely to self-report a recent URTI than those with sufficient levels 13
. These findings where consistent when adjusting for variables including season, age, gender, body mass, race. In another cross sectional study involving 800 military recruits in Finland. Those recruits with lower vitamin D levels lost significantly more days from active duty secondary to URTI. It is worth mentioning that studies reporting potential benefits of administering vitamin D to decrease infections have not been consistent. Nevertheless, a well-designed prospective double blind placebo used nasopharyngeal (nose and throat) swab cultures and a therapeutic dose of vitamin D showed that the administration resulted in a statistically significant (42%) decrease in the incidence of influenza infection 14
. The beneficial effects of vitamin D on protective immunity are due in part to its effects on the innate immune system. Vitamin D plays an important in the innate antimicrobial response. The necessary vitamin D to meet these levels of protection can be obtained through supplement, sunlight above all dietary intake.
Dietary intake along with the aforementioned acute exercise not only manages weight management and obesity, but also provides a noticeable boost to the immune via the diversity of the gut microbiota. The gut microbiota influences human health and immune function, though fermentation of indigestible food components in the large intestine. The microbiome and derived metabolites include short chain fatty acids and biotransformed bile acids have been shown to influence immune function both within the gut and systematically. However, it is worth mentioning that research in this area is emerging and more needs to be done to determine potential linkage between immune function in physically fit individuals. Nevertheless, consuming a well-balanced diet with sufficient energy to maintain a healthy weight, with a focus on grains, fruits and vegetables to provide sufficient carbohydrate and polyphenols that reduce exercise-induced inflammation and improve viral protection, is thoroughly recommended.
Finally, lifestyle is the last holistic approach and the most impactful on the maintenance of and fortification of an effective immune system in an individual. These lifestyle recommendations adhere to consistently overtime, become positive daily habits. These lifestyle recommendation include facilitate regular high quality sleep avoid excessive intake of alcohol, consume a well-balanced diet and the development of stress management and copying techniques to decrease load of life hassles, stress, negative life events and emotions. Numerous studies have revealed that sleep deprivation reduces the levels of cytokines, infection fighting antibodies and cells. The consequences of this is that it makes the body less responsive to vaccines an consequently this has a profound on antiviral immune response 15
.
With regards to alcohol, its combined effects on both innate and adaptive immunity significantly weaken host defences predisposing chronic drinkers to a wide range of health problems including infections and systemic inflammation 16
. More pertinently to COVID-19, alcohol disrupts ciliary function in the upper airways impairs the function of immune cells (i.e. alveolar marcophages and neutrophils), and weakens the barrier function of the epithelia in the lower airways. Often, the alcohol-provoked lung damage goes undetected until a second insult, such as respiratory infection leads to more severe lung disease than those seen in non-drinkers 17
. Also alcohol alters the number of relative abundances of microbes in the gut microbiome, these organisms affect the maturation and function of the immune system.
The effects of stress, emotional trauma on the immune system are well documented. Studies have shown that stress is responsible for immunological dysregulation in children, adolescence and adults alike, which presents with an increase blood levels of pro-inflammatory cytokines and even more so with chronic stress. In addition to this chronic stress is activation of latent viruses. Latent virus activation can reflect the loss of immunological control over the virus and frequent activation can cause wear-and-tear on the immune system.18
In conclusion, the hoslitic approaches adopt the most effective strategy and something all healthcare professional prescribe to the public, prevention. Only through prevention can COVID-19 be well managed and contribute to the fatalities attributed to this virus. To reiterate these holistic measures are easy to incorporate into our daily lives, they are relatively inexpensive and so present a low barrier to adopt and they are indeed highly effective in preventing the spread of the virus. Adhering to these measures makes a serious effort and contribution towards reducing the pressure on NHS resources both financially and emotionally. What’s more, complying with hygienic & social practices in the form of wearing a mask and regularly hand washing are fitting and meaningful acts we can undertake to show our appreciation for and solidarity with NHS workers, key workers and each other. In the final part of this series, we shall look at the proposed vaccine and therapeutic options used to combat the virus.
© All rights reserved, Nnadi’s Healthcare & Pharmaceuticals Limited, 2020.
Reference
1. P Thordarson. The coronavirus is no match for plain, old soap – here’s the science behind it. MarketWatch. <https://www.marketwatch.com/story/deadly-viruses-are-no-match-for-plain-old-soap-heres-the-science-behind-it-2020-03-08> Accessed 30th August 2020.
2. V Curtis S Camicross. Effect of washing hands soap on diarrhoea risk in the community: A systematic review. Lancet Infect Dis. 2003;3(5):275-81.
3. T Rabie V Curtis. Handwashing and risk of respiratory infections: a quantitative systematic review. Trop Med Int Health. 2006; 11(3):258-67.
4. WHO. Mode of transmission of virus causing COVID-19: Implications for IPC precaution recommendations <https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations> Accessed 27th August 2020.
5.BBC News. Coronavirus: Face covering use expanded in England and Scotland. <https://www.bbc.co.uk/news/uk-53702291> Accessed 27th August 2020.
6. J Henley. Global Report: France tightens mask rules as Covid cases rise in Europe. The Guardian. <https://www.theguardian.com/world/2020/aug/18/global-report-france-tightens-mask-rules-as-covid-cases-rise-europe> Accessed 30th August 2020
7.Ibid 4
8. S Whitebloom. Social distancing works: Here’s the Maths. Oxford Science Blog. University of Oxford. <https://www.ox.ac.uk/news/science-blog/social-distancing-works-here-s-maths> Accessed 27th August 2020.
9. DC Nieman LM Wentz. The compelling link between physical activity and the body’s defense system. J Sport Health Sci. 2019; 201-217.
10. Ibid
11.S Boseley. Obesity increase risk of Covid-19 death by 48%, study finds. The Guardian.<https://www.theguardian.com/world/2020/aug/26/obesity-increases-risk-of-covid-19-death-by-48-study-finds> Accessed 29th August 2020.
12. C Aranow. Vitamin D and the Immune System. J Investig Med. 2011;59(6):881-886
13. AA Ginde JM Mansbach CA Camargo Jr. Association between serum 25-hydroxyvitamin D level and upper respiratory tract infection in the Third National Health and Nutrition Examination Survey. Arch Intern Med. 2009; 169(4):384-90.
14. M Urashima et al. Randomised trial of vitamin D supplementation to prevent seasonal influenza A in schoolchildren. Am J Clin Nutr. 2010; 91(5):1225-60.
15.MR Irwin. Why Sleep is important for Health: A Psychoneuroimmunology Perspective. Ann Rev Psychology. 2015; 66:143-172
16. D Sarkar MK Jung H Joe Wang. Alcohol and the Immune System. Alcohol Res. 2015; 37(2):153-155.
17. Ibid.
18. JN Morey IA Boggero AB Scott SC Segerstrom. Current Directions in Stress and Human Immune Function. Curr Opin Psychol. 2015; 5:13-17

Following on from our “Faith & Medicine” article and in keeping with the theme of spirituality, I’d like to announce that the Archangel Michael stands as the patron of Nnadi’s Healthcare & Pharmaceuticals Ltd. “St Michael the Archangel, defend us in battle, be our protection against the wickedness and snares of the devil. May God rebuke him we humbly pray; and do thou, O Prince of Heavenly host, by the power of God, cast into hell Satan and all evil spirits who prowl about the world seeking the ruins of souls.” Whilst Nnadi’s Healthcare & Pharmaceuticals remains a company that will always stay true to the principles of evidence-based medicine and “Good Science”, we pledge to utilise the scientific skill, talent and ambition that this company possesses to best serve patients & customers be they in the United Kingdom or abroad. Our privilege to serve those in need of our goods & services is a commitment we do not take lightly. We are most humbled and grateful to undertake this responsibility, and thus ask for the guidance & protection of St Michael the Archangel in all our endeavours henceforth. Most Sincerely, Sonny A. Ume Founder & Managing Director

In the Western world, and specifically to Western medicine (allopathic medicine), faith commonly tends to meet medicine at the intersect of “last resort”. Sporting analogies vividly depict such dire occasions, the “Hail Mary Pass” of American Football, “The bottom of the ninth” of American baseball or “90 minutes plus stoppage time” in football (soccer). Once the game plans and tactics have been tried and exhausted to no avail, the game of the respective sports take on a more urgent, opportunistic and hopeful complexion for the teams involved. This scenario is very much reminiscent of when medicine has been deployed as the opening gambit to tackle ill health only to find it is yielding little to no dividends towards improving to the patient’s health or condition. In this situation desperate times call for desperate measures and in the face of such desperation faith is sought and clung onto. Faith and medicine enjoy a polarising duality; Spirituality versus Science, “The Unseen” versus “The Proven”, subjectivity versus objectivity, belief versus evidence. Even in the face of this presented incompatibility between Faith and Medicine, there resides a common thread that unifies both. Patients. This article will look at the importance of acknowledging faith in medicine and the role faith plays in healthcare, particularly in primary care. The opening sentiment of this article on the relationship between Faith and Medicine may appear somewhat flippant and reductive. For some patients, faith does not follow a sense of hopelessness or vulnerability. Rather faith, in their respective religion, is their North Star. Their compass in navigating their day-to-day life of which, their healthcare needs are no different. Faith is central to the identity of an individual and for the collective community and demographic. An understanding of a patient’s faith in the healthcare sector is necessary in a multicultural country like the UK and more so in her multicultural major cities such as London. According to the latest data from the ONS (Office for National Statistics) 2021 Census, Christianity remains the largest religion in London with 40.66%, with Islam, Hinduism, Judaism, Sikhism and Buddhism following in sequential order at 14.99%, 5.15%, 1.65%, 1.64% and 0.99% respectively 1. When making an eyeball comparison of the religions distribution chart from the ONS 2011 Census against the ethnic group distribution chart from the 2021 Census, it provides a quantitative and qualitative insight into where specific demographics are situated across London 2. For instance you will find a majority of the Black Afro-Caribbean demographic in South East London an area with a high number of individuals identify as Christians, Asian-Indian in West London, an area where a large majority identify as Hindus and Sikhs, Asian Pakistanis far West & East London where Islam is the dominant religion and individuals who identify as Jewish are predominantly situated in the North and North West London area. A majority people who identify within an ethnic group demographic will have some connection to a religion, which plays an integral part to shaping their culture as well as their faith. This is of significance as these individuals then to be those as risk of preventative chronic disease of which the health outcome can be a poor prognosis. The data derived from the charts below will form the basis for strategies that are to be deployed in meeting the clinical needs of the multicultural demographic in London.

Dear Reader, We’d like to apologise for our absence and inconsistency in our posting activities. We had planned for 2023 to be the year to springboard growth for the company. However, by August 2023 our plans were derailed by unapproved amendments to an investment deal, unforeseen operational changes by appointed service partner and the negligent damage to our current stock. Due this catalogues of disruptions, it resulted in the business having to concentrate its efforts on stabilizing and navigating through this thorny period. Sadly the decisive actions we took have impacted our agility and growth for 2023 heading into early 2024. It would be no stretch of the English language to deem 2023 as an annus horribilis for Nnadi’s Healthcare & Pharmaceuticals. Despite the hurdles of learning and operational obstacles to surmount, we persevere not out of foolishness or folly but out of a sense of duty and determination to contribute something positive to the country. Something positive for the nation’s economy and the health of the population too. Through Fergie’s Sparkling Water®, we have had the opportunity to connect and listen to people. We have come to gain an insight into people’s relationship with their nutrition, GP and the NHS as a whole. Through these conversations with the public, it is apparent there is still much work to do. Aside from these conversations, I would be remiss not to mention and acknowledge the kind words of support and gradual return business we have accrued in spite of all these difficulties since August 2023. We are grateful to these customers and supporters, we shall repay their faith by continuing to make strides towards securing investment. Our path towards securing investment now adopts a strategy of patience (as much as we can afford). The investment climate in the UK is constricted and conservative to nascent SME science ventures. According to an experienced business advisor, investments in the UK have dropped by 61%. Aside from the slow velocity of investment capital, there seems to be a shortage of courage and patience towards modest & sustainable business model. Investing in STEM ventures is not for the faint-hearted, but it is an investment that pays dividends both financially and socially. In this climate, we have to wait discerningly for the correct investing partner that will pull us out of the vicious cycle of traction against capital. I have full confidence in the company’s potential and mission. I hope this is a sentiment shared by our investors. We shall indeed wait and see. In the meantime, we shall continue with our daily operational activities and ambitions. We have come to accept that investment is very much now a waiting game. Kindest Regards, Sonny Ume Founder & Managing Director

Dear Reader, This year has been a year of marked progess and incremental growth in comparison to the previous year. Early into Q1, we began officially trading with Fergie’s Sparkling Water ® and have been garnering sales throughout the year. Between late Q2 and mid Q3 , we encountered challenges and hinderances in involving our marketing campaign impeding us from fully capitalising upon the double heatwave that swept through the UK in the Summer. Due to thte unwelcomed impact, we have parted ways from the responsible marketing firm that oversaw our campaign during the periods of the aforementioned quarters. New marketing partners have been identified for 2023. Despites seeing sales and an increase in social media follwers across all platforms, we have had to contend with difficult macroeconomic factors. The leading macroeconomic factor has indeed been the steep rise in inflation, exacerbated by the Russia-Ukraine conflict in March of this year leading to soaring commodity prices affecting businesses, families and individuals alike. As a result of this, the UK, amongst other countries in Europe, are enduring a cost of living crisis. In relevance to our sector, for Fergie’s Sparkling Water ® , grocery shopping (food) inflation currently stands at 14.6% (down 0.1%, 6 Dec 2022), significantly higher than this time last year’s recorded at 4.2%. To combat this inflationary environment we have decided on two courses of action. Firstly, we have opted not to engage in cost-push inflatuion from our end, which would see us pass the additional cost onto the consumer. This is clearly demonstrated by us not levying a delivery charge on the customer’s orders. Secondly, we have offered small sample packs and have revised and reduced our prices across our current SKU (flavours/lines) which now includes multiflavour packs. These practices have created new customers, returning customers and prospective customers. Regarding the later, we have seen an increase in orders left at the basket checkout (a common practice observed by e-commerce merchants and retailers). We would prefer to convert these incompleted orders to sales. We shall indeed concentrate attention and focus on this practice and these prospective customers in the coming year. Aside from opening achievements and current challenges, we have achieved milestones on a marketing and parternship front this year. In mid Q2 we were part sponsors of a well known health conference with leading dietician and nutritionist . We will explore the possibility of sponsoring this event again. In addition to this come Q1 of 2023 we will be sponsoring a University Netball Team Club for the second half of their season. We intend for this to be a promising promotional endeavour. Whilst forming sponsorship links we enagegd in our first out-of-home (OOH) marketing campaign in a thriving and bustling area within the city of London. This achievement and opportunity allowed us for to showcase our distinctive golden cans and unique and delicious flavours to passers-by in the capital. Again, we aim to incorporate this form of marketing into future marketing campaigns. Rounding up on positive fronts, the final preparations are being made towards the end of Q4 following the better articulation of our product portfolio and strategy heading into 2023. On behalf of the company I am filled with much confidence and optimism as to what lies ahead for 2023. Overall, 2022 has provided an additional 12 months that have served as an invaluable learning curve. Both in evaluation and identification and better yet, realization. And come the end of this year we realize the necessity and central importance of securing funding in 2023. I believe my confidence and optimism are not misplaced surrounding the current potential and awaiting achievements of this company. For, if we can successfully complete our next round of funding and secure sufficient capital investment, it would serve as both fuel and vehicle to propel our commercial ambitions and endeavours. Nnadi’s Healthcare & Pharmaceuticals aspires to make its contribution to the gauntlet and satellite challenges that have arisen following the aftermath of the COVID-19 pandemic and subsequent scrutiny of the pharmaceutical industry. Given our stance towards the current perception of the pharmaceutical industry and our intended efforts to a propose remedy to the heightened scrutiny through Nnadi’s Healthcare & Pharmaceuticals’ operating model, hence there has not been a more enticing time to be involved in this sector. Nnadi’s Healthcare & Pharmaceuticals will strive to be among those enterprises, big and small, who wish to use all their efforts in tackling the challenges and seizing the opportunities that lie ahead in this field. Again, our ambition can only be realized with the necessary capital to fortify and grow based on what we have achieved so far. In closing, and returning to current matters, I would like to take this time to thank you for reading this and subsequent articles we have posted this year. I would like to thank all those who have supported and offered advice to bring us this for. And finally, above all else I would like to thank our customers who have invaluable not just in support through purchase, but in patience too. I would like to wish you and you a very Merry Christmas and a happy and prosperous New Year. May 2023 be a year of achivements and delivery for you as I hope it will be for Nnadi’s Healthcare & Pharmaceuticals. Kind Regards, Sonny Ume Founder & Managing Director Nnadi’s Healthcare & Pharmaceuticals Ltd.

Fergie’s Sparkling Water ® is delighted to announce it will be a sponsor for the second half of the University of Strathclyde Female Netball Club (USFNC). Fergie’s Sparkling Water ® can be enjoyed as part of a healthy diet, but as a thirst-quenching healthier alternative after physical activity such as sports. Increasing and encourage physical activity, through the medium of sports, is something we wish to do now and in the future. A club officer and player of the USNC, Oriana Smith said; “We have chosen Fergie's Sparkling water as one of our sponsors this year because we really believe in their product of a healthy alternative to sugary soft drinks. As a netball team who take our sport seriously, we can't wait to enjoy Fergie's drinks after our games and around Strathclyde Campus. Thanks so much Fergie's for being one of our sponsors this year!” We will certainly cheering the team on!

The pharmaceutical industry is a force for good! Our opening remark serves as a reminder and maxim within our company’s mission statement of elevating the patient’s and consumer’s perception of the pharmaceutical industry. Now more so than ever in recent times, this maxim of ours is necessary to recalibrate the perception of our industry. For failure to do so will have far reaching consequences, not just upon the pharmaceutical industry but also on public health. As it stands, Big Pharma and the remaining stakeholders within the pharmaceutical industry must, if not currently are, run through a gauntlet consisting of disenfranchised, incredulous and angry members of the public. This brief will look at the current obstacles and challenges that await Big Pharma and other industry players, whilst proffering solutions that go some way to repairing the strained relationship between pharma and the public. The objective of this reconciliation between both pharma and public seeks to restore the lack of confidence and subsequently the trust that has been broken. The future and integrity of the pharmaceutical industry depends on the mending of this relationship. Beginning with confidence itself, it is its latter crystalised end product of trust, that has been eroded or completely shattered resulting in the pharmaceutical industry being brought into disrepute. The leading contributing factor has been the lack of transparency in commercial activities and the decisions of Pfizer Inc. surrounding their vaccine. The earliest sense of opacity and perceived artifice involved the non-attendance of Albert Bourla pulling out of an initially scheduled European Parliament’s special committee on COVID (COVID committee). Mr. Bourla was not legally bound to attend nor was he subjected to any criminal punishment, as this was not an inquiry. Mr Bourla was intended to speak off the record. Mr. Bourla’s non-attendance proved irksome and did little to quell the committee’s frustration in the pursuit of answer. Another invitation has been extended to Mr Bourla. In Mr. Bourla’s place Janine Small, Pfizer’s Regional President of International Developed Markets stood in. The committee sought to address their concerns surrounding the heavily redacted vaccine purchase contract and the text messages between the Pfizer CEO and EU President Ursula von der Leyen. French MEP and COVI Committee member Veronique Trillet-Lenoir put these questions to Ms. Small. The purpose of Ms. Trillet-Lenoir’s line of questioning was to establish the relevant components about the operations in the manufacturing and delivery of the vaccines. 1 To this, Small answered that the information remains confidential for “competition reasons. This answer in the eyes of the COVI Committee ran contrary to Pfizer’s initial claim of transparency.

The role of a mother in the development of an infant is invaluable. Whether it be supporting intellectual development or social development at an early age, there remains and even more crucial form of development. Nutritional development. To mark the significance of nutritional development in the early weeks and months of a babies’ life, the first week of August (1st-7th) is considered World Breastfeeding Week by the World Alliance for Breastfeeding Action (WABA). WABA is a global network of individuals and organisations dedicated to the protection, promotion and support of breastfeeding worldwide. However, it would seem that the message and rationale promulgated by WABA faces much challenge whilst heading towards a collision course with the proprietors of instant baby formula milk (IBFM) a form of breast milk substitute (BMS) and their proliferation over the previous decades. This article will explore how and whether the marketing practices deployed to promote BMS affects and hence jeopardises breastfeeding. We shall look at the importance and significance of breastfeeding, the current challenges and barriers to breastfeeding. We’ll review the marketing practices used by brand labels of IBFM and rebuttals they propose to these claims. Finally, we shall conclude on the repercussions of these claims on the marketing practices and their impact on breastfeeding and IBFM, before providing a conclusion. Breastfeeding is one of the earliest and vital acts a mother engages in to support the physiological and nutritional development of her baby. It is for this reason why the World Health Organisation (WHO) recommends solely breastfeeding babies for the first six months of their life. 1 The WHO’s recommendation stems from the constituents of human breast milk, all of which contain basic essential nutrients such as carbohydrates, protein and fats too. Apart from breast milk being tailor made for a mother’s baby, breast milk is rich in million of live cells (white blood cells and stem cells etc.) that are immune-boosting and help organs develop and heal. Breast milk contains enzymes, growth factors, antibodies known as immunoglobulins (key in protecting the baby from illness and infections) by neutralising bacteria and viruses. In addition to this breast milk includes long-chain fatty acids, which play a pivotal part in the development of a babies nervous system, brain and eye development. Finally, breast milk contains 1,400 microRNAs which are thought to regulate gene expression crucial in preventing or halting disease development, whilst supporting the babies immune system and remodeling of the mother’s breast. 2 The development and properties of breast milk occur over three stages; colostrum, transitional milk and mature milk (foremilk & hindmilk).

Inflation, defined in simple economic terms, is when prices of goods and services generally increase (along with a rise in demand) whilst reducing the purchasing power of money as each unit of currency buys fewer goods and services. The 40th President of the United States, Ronald Reagan, once quipped, “Inflation was violent as a mugger, frightening as an armed robber and as deadly as a hit man.” And as this perpetrator is very much on the loose and as of the time of writing, poses a clear and present danger to family and households in the West. The global economy, in particularly those of the West, is emerging from the embers and effects of the COVID-19 pandemic and whilst still undergoing a jittery and steady recovery, inflation seems to have stalled and in some cases reverse growth in the West. In the United States inflation has hit an annual rate of 8.3% down from 8.5% in March, but still an inflation rate that remains close to a 40-year high.1 Across the pond, Western European nations are grappling, with inflation across the Eurozone reaching 7.5%.2 In addition to this, the raging conflict between Russia and Ukraine has exacerbated the inflationary pressures on the continent. This article will look at how inflation is impacting the UK population and the dangers towards diabetes prevention and what attainable steps or measures can be taken to tackle this. Despite the backdrop of the COVID-19 pandemic, the escalation of geopolitical tension between the US, Russia and Ukraine has now regrettably broken out into military conflict as of Thursday 24th February 2022 and has sent commodity prices soaring. As of 2019, Russia and Ukraine exported more than 25% of the World’s wheat.3 Ukraine is considered the breadbasket of Europe, as 71% of Ukraine land is agricultural. Ukraine is also home to a quarter of the World’s “black soil” or “Chernozem”, which is highly fertile.

“Be yourself” , “Love who you are” and “Never apologise for being you” are common self affirmations associated with wellbeing but can extend to body positivity. The fashion, beauty and sporting industry are leading the vanguard on the encouragement of body positivity in the name of representation and diversity of body types. This is indeed a good thing and very much welcomed. However, there must be a sense of awareness and caution to the indirect promotion of any health implications, in particularly prediabetes. This article will explore the dichotomy between social norms of body positivity versus clinical (health) concerns surrounding body positivity. This article will cover, to an extent, the relationship and impact of body positivity and body image may have upon mental health, healthy weight management and how best to beat prediabetes and Type-2 diabetes. Finally, we shall cover how a healthy weight is calculated, its significance and metabolic difference between individuals. This article will not cover nor engage in any post-discussion or debate on the topic of body positivity in relation to attraction. From a medical viewpoint, attraction is a subjective, fickle and not germane to this article. Given the sensitivity of the subject it would be appropriate to cover the impact on mental health and psychological well-being. Body positivity is inextricably linked to our self-image, which is key to our sense of identity. Simply put, how we look equates to how we feel. The perpetuation and desirability in the pursuit of the “perfect body” arises primarily from various forms of consumption. Common sources and outlets of this category include; Hollywood, Reality TV, ITV’s mega-successful Love Island franchise and Meta’s Instagram, all offering a window into innocuous entertainment, whilst showcasing the latest beauty trends that go on to become the societal standard. However, this harmless form of entertainment ceases to be so when the perpetuated trends by A-listers, well-known celebrities or recognised public figures (devoid of malice or agenda on their part), are, perceived as unattainable. It is this realisation that is impactful and leaves a detrimental effect on the most vulnerable members of the public on the uses of body image- teens and adolescents. The data to support this is worrying. According to UK survey of 11-16 years olds conducted by Be Real found that 79% said how they look is important to them. Over half (52%) often worried about how they looked. 1 In a survey of young people aged 13-19, 35% said their body images cause them to ‘often’ or ‘always’ worry. Research has shown that girls are more likely to be dissatisfied with their appearance an their weight than boys.2 3 In a survey by Mental Health Foundation, 46% of girls reported that their body image caused them to worry ‘often’ or ‘always’ compared to 25% of boys.4 In addition to this UK survey by Be Real, targeted at UK adolescents, it was revealed that 36% agreed they would do whatever it took to look good with 57% saying they had considered going on a diet and 10% saying they had considered cosmetic surgery.5 Disturbingly among secondary school boys, 10% said they would consider taking steroids to achieve their goals.6 Through these surveys, young people have expressed that body image is a substantial concern. Body satisfaction and a pressure to be thin is linked to depressive symptoms such as anxiety disorders (social anxiety or panic disorder) particularly in those children who do not match societal views of the ideal body.7 8 9 Possessing a poor body image may also prevent young people from engaging in healthy behaviours, as studies have found that children with poor body image are less likely to take part in physical activity. Survey data has shown that 36% of girls and 24% of boys avoided taking part in activities like physical exercise/physical education (P.E.) due to worries about their appearance. Body image is a substantial concern identified by 16-25 year olds and is the third biggest challenge currently causing harm to young people behind a lack of employment opportunities and failure to succeed within the education system being the first two.10
To mark the Diabetes (Type-2) Prevention Week, we shall provide you with a brief overview of what prediabetes is, why it is significant, who is most at risk and what can be done to tackle it. What is prediabetes? Prediabetes, also known as non-diabetic hyperglycaemia, is a serious health condition that sees a person’s blood glucose level reside above the healthy range, but reside just below the range required for the person to be diagnosed with Type-2 Diabetes (T2D). An individual is deemed prediabetic if they have an HbA1c reading of between 42mmol/mol (6%) to 47.9mmol/mol (6.4%) or a fasting plasma glucose (FPG) of 5.5mmol/l to 6.9 mmol/l. In the UK, statistics suggest that there are 13.6 million people at risk of developing Type-2 diabetes.